Post-Stroke Care and Rehabilitation in Kathmandu: A Clinical Guide to Recovery and Ongoing Support
A stroke arrives without warning, but its consequences unfold over months and often years. For survivors and their families in Kathmandu, the period after hospital discharge can be confusing and emotionally demanding. Acute treatment saves life, but recovery depends on what follows. Post-stroke care and rehabilitation are not optional extensions of treatment. They are the core of long-term recovery.
In Nepal, where families often play a central role in caregiving, structured post-stroke support becomes even more important. Recovery is rarely linear. Progress may be slow, uneven, and at times frustrating. With appropriate rehabilitation, consistent medical follow-up, and realistic guidance, many stroke survivors regain meaningful function and stability. This guide explains post-stroke care from a clinical perspective, with practical relevance for patients and caregivers in Kathmandu and surrounding areas.
Understanding Stroke and Its Long-Term Effects
A stroke occurs when blood flow to part of the brain is interrupted. Ischemic stroke, caused by a blocked artery, is the most common type seen in Nepal. Hemorrhagic stroke, resulting from bleeding in or around the brain, is less common but often more severe. In both cases, damage occurs because brain tissue is deprived of oxygen.
The effects of stroke depend on which area of the brain is affected and how quickly treatment begins. Many patients experience weakness or paralysis on one side of the body. Speech and language difficulties are common, as are problems with balance, coordination, memory, and attention. Emotional changes such as depression, anxiety, irritability, or loss of motivation are frequently under-recognized but clinically significant.
Post-stroke care and rehabilitation are designed to address these consequences in a structured way, supporting the brain’s capacity to adapt while helping patients adjust to lasting changes when full recovery is not possible.
The Importance of Early Rehabilitation
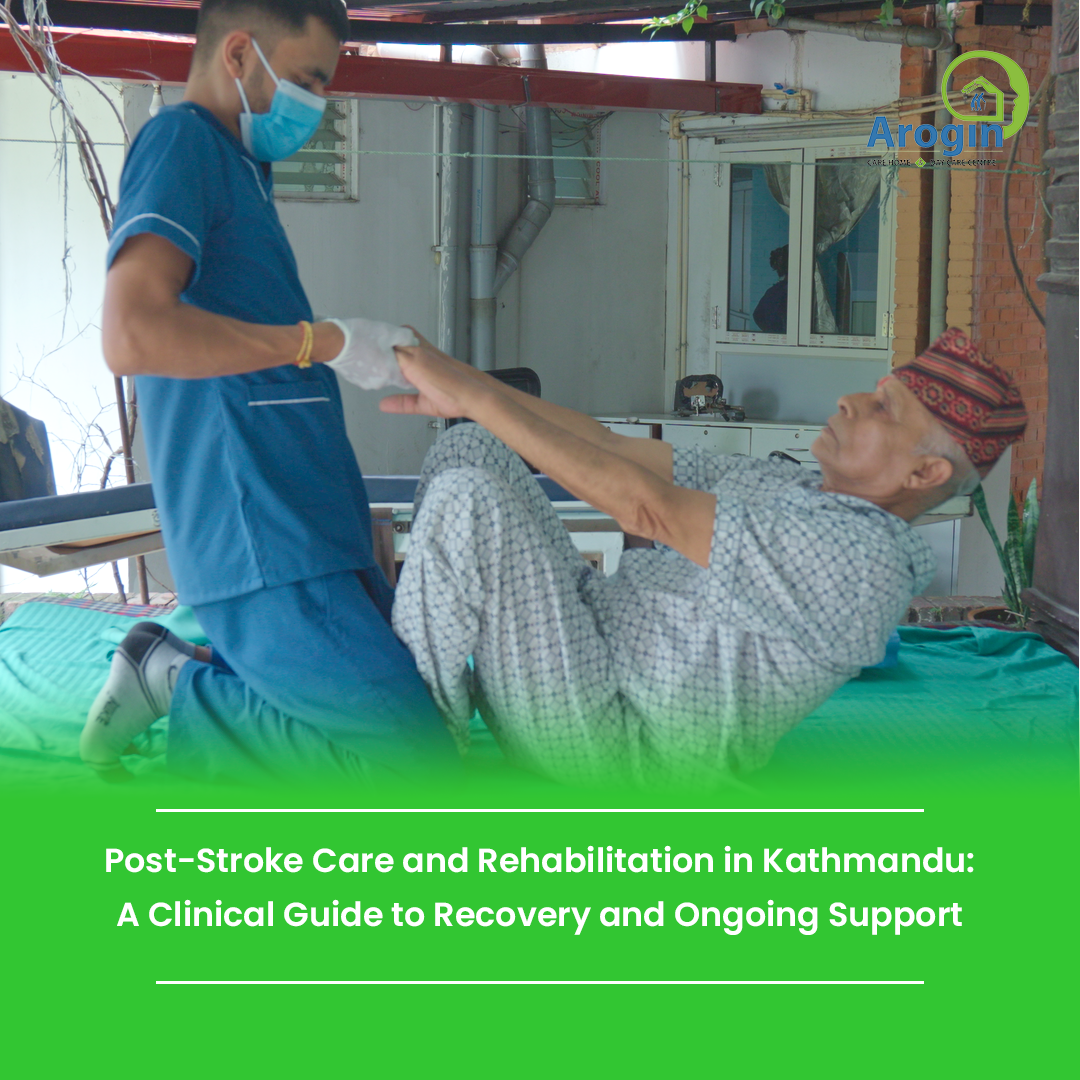
Rehabilitation should begin as soon as the patient is medically stable. In clinical practice, early mobilization and therapy reduce complications such as joint stiffness, muscle wasting, pressure injuries, and respiratory problems. Just as importantly, early rehabilitation helps patients regain confidence at a time when fear and uncertainty are common.
Evidence consistently shows that the first weeks after stroke are a critical window for recovery, but improvement does not stop there. Many patients in Kathmandu continue to benefit from rehabilitation months after the initial event, especially when therapy is adjusted to their progress and living environment.
Facilities such as Arogin Care Home work with this longer timeline in mind, focusing not only on early gains but also on sustained functional improvement and safe long-term care.
Key Components of Post-Stroke Rehabilitation
Effective post-stroke care requires coordination between medical professionals, therapists, patients, and families. No single therapy addresses all needs. A multidisciplinary approach allows rehabilitation to remain practical and patient-centered.
Physical Therapy After Stroke
Physical therapy focuses on restoring movement, strength, balance, and coordination. After a stroke, muscles may be weak, tight, or poorly controlled. Physical therapists guide patients through exercises that retrain basic movements such as sitting, standing, and walking.
Therapy often includes stretching to manage spasticity, strength training to rebuild endurance, and balance work to reduce fall risk. Progress is gradual. Clinically, small improvements such as safer transfers or improved walking stability can significantly improve independence.
In Kathmandu, where uneven terrain and stair use are common, therapy must be adapted to real-life mobility challenges rather than ideal clinical settings.
Occupational Therapy and Daily Function
Occupational therapy addresses how neurological deficits affect daily activities. Tasks such as dressing, bathing, eating, or writing can become difficult even when muscle strength appears adequate.
Occupational therapists help patients relearn fine motor skills, adapt techniques for daily tasks, and use assistive devices when appropriate. Home safety assessments are particularly important in Nepalese households, where space constraints and floor-level living can increase fall risk.
Regaining independence in daily activities often has a greater impact on quality of life than isolated physical improvements.
Speech and Swallowing Therapy
Speech and swallowing difficulties are common after stroke and require careful evaluation. Speech-language pathologists address problems with speech clarity, language comprehension, reading, writing, and cognitive communication skills such as attention and memory.
Swallowing disorders are a serious medical concern. Therapy focuses on improving safety during eating and drinking to reduce the risk of aspiration and related complications. Improvement in communication often leads to better social engagement and emotional well-being, which are essential for long-term recovery.
Cognitive and Emotional Rehabilitation
Stroke frequently affects cognitive function and emotional regulation. Memory problems, reduced concentration, poor planning, and emotional instability can interfere with daily life and strain family relationships.
Cognitive rehabilitation includes structured exercises and practical strategies to compensate for deficits. Emotional support may involve counseling, psychological therapy, or guided family education. Depression and anxiety are common after stroke and should be addressed with the same seriousness as physical symptoms.
At Arogin Care Home, emotional and cognitive health are considered essential components of post-stroke care rather than secondary concerns.
Post-Stroke Care at Home in Nepal
Returning home is a major transition. In Kathmandu, where family members often serve as primary caregivers, stroke care at home requires planning and shared responsibility. A consistent daily routine helps patients feel secure and reduces confusion. Encouraging independence, while ensuring safety, supports both recovery and dignity.
Caregivers assist with prescribed rehabilitation exercises, medication schedules, and follow-up appointments. Simple adjustments such as improving lighting, reducing clutter, or installing handrails can significantly reduce fall risk.
Caregiver fatigue is common and often overlooked. Long-term care is demanding, and caregivers benefit from professional guidance, respite options, and emotional support.
Lifestyle Factors and Stroke Prevention
Lifestyle management is part of post-stroke care, not an afterthought. A balanced diet, appropriate physical activity, and regular monitoring of blood pressure, blood sugar, and cholesterol are essential to reduce the risk of another stroke.
Smoking cessation, limiting alcohol intake, adequate sleep, and stress management all support neurological recovery. These measures are particularly relevant in urban settings like Kathmandu, where sedentary routines and unmanaged hypertension are common contributors to stroke risk.
Common Challenges During Recovery
Stroke recovery is unpredictable. Fatigue, slow progress, emotional frustration, and temporary setbacks are normal. Financial constraints and limited access to ongoing therapy can also affect rehabilitation continuity in Nepal.
Understanding that recovery is not linear helps patients and families maintain realistic expectations. Open communication with healthcare providers allows care plans to be adjusted when progress stalls or new challenges arise.
How Long Does Post-Stroke Recovery Take?
There is no fixed timeline for recovery. Many patients experience the most noticeable improvement within the first three to six months, but continued gains are possible well beyond that period. Age, stroke severity, pre-existing health conditions, and consistency of rehabilitation all influence outcomes.
Life after stroke often involves adaptation rather than complete restoration. Learning new ways to perform daily tasks can be just as important as regaining lost abilities.
When Ongoing Professional Support Is Needed
Medical and rehabilitative follow-up remains important throughout recovery. New symptoms, sudden functional decline, or worsening emotional distress require reassessment. Caregiver strain is also a valid reason to seek additional support.
Facilities providing structured long-term care, such as Arogin Care Home in Kathmandu, can play an important role when home care alone is no longer sufficient or sustainable.
Frequently Asked Questions
What is post-stroke care and rehabilitation?
It involves medical management, physical and cognitive therapies, emotional support, and lifestyle guidance to help stroke survivors regain function and stability.
Can stroke patients fully recover?
Recovery varies. Some regain most functions, while others live with lasting limitations. Rehabilitation focuses on maximizing independence and quality of life.
Are rehabilitation exercises necessary at home?
Yes. Home-based exercises help maintain and extend progress made during therapy sessions.
How can families support recovery?
Families support recovery by encouraging consistent therapy, providing emotional reassurance, ensuring medication adherence, and maintaining a safe living environment.
Is emotional recovery part of stroke rehabilitation?
Yes. Emotional and cognitive health are integral parts of comprehensive post-stroke care.
Moving Forward After Stroke
Recovery after stroke is a long process shaped by patience, consistency, and support. Post-stroke care and rehabilitation provide a structured path forward, addressing physical, cognitive, and emotional needs together. Progress may be slow, but it is often meaningful.
For patients and families in Kathmandu navigating life after stroke, informed guidance and reliable care make a measurable difference. Recovery does not happen in isolation. Each step forward reflects coordinated effort, professional support, and sustained commitment over time.